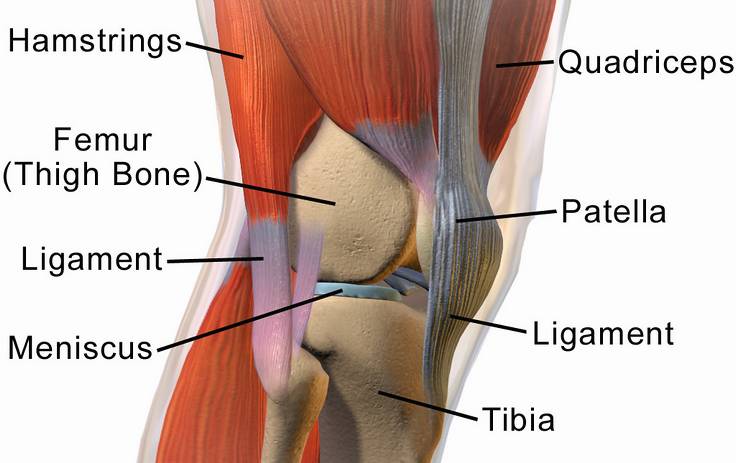
Your knee takes a substantial force when walking and many times your body weight when running. The movement this remarkable structure provides can be affected by wear, by a sudden blow, by twisting, or turning.
Symptoms of patella (kneecap) dysfunction will vary. Your kneecap may slip to the side of the joint and feel out of position, pain can come with movement, tenderness and swelling be evident, or you may have a problem with straightening your leg.
Dislocation can also bring a catching,or giving way sensation, or creaking sounds but so can damage to a cartilage (meniscus) along with clicking, or grinding.
Knee symptoms are interlinked and damage to one aspect may affect others. Kneecap dislocation can cause cartilage damage and may cause injury to the ligament which holds it in place.
Individual Diagnosis
Careful diagnosis is essential to identify the areas affected by wear and tear, or injury. This may require a visit to the imaging suite for an MRI scan, a process which has revolutionised diagnostic accuracy for knee injuries.
A detailed consultation will follow, where an orthopaedic specialist can consider your specific injury and wider medical implications.
Their objective is to restore smooth, friction free movement. Ensuring that all damage is understood is important, to allow a detailed treatment plan to be created.
There are times when knee injuries can be treated in non surgical ways, such as cortisone injections combined with physiotherapy. They will be explored, although for a significant injury, surgery may be the best option.
Treating Patella Dislocation
The patella sits in a groove in the femur and is held in place by the medial patellofemoral ligament (MPFL), which attaches to both bones. The MPFL may be torn or stretched as part of dislocation, or a previously damaged ligament can lead to recurrent dislocations.
In cases where dislocation has not caused further injury, putting the kneecap back in place and good support from a physiotherapist may suffice. Where there is wider damage, work on the cartilage or the MPFL may be needed.
A new technique to treat MPFL tears has been developed over the last decade, called MPFL reconstruction. This involves the use of a hamstring graft, or an augmentation device called an internal brace, which stabilises and strengthens the kneecap.
Cartilage Tears and Defects
Treatment for cartilage tears has advanced in recent years. In younger patients (under 40) this can often be managed through cartilage repair using keyhole surgery, rather than debridement (removing tissue).
This may be an effective medical approach, which also allows for an improved functional recovery and can delay the development of post-traumatic arthritis.
Cartilage defects for all ages can be managed using a transplant approach, called osteochondral autograft transplantation system (OATS). Occasionally, a nanofracture technique is used, where bone marrow and stem cells are encouraged to stimulate regrowth.
Individual Support
Defining the exact nature of any issues you have with your knee is the basis of good care. We would encourage you not to ignore knee injuries or discomfort, which may have readily treatable underlying causes.
Ongoing instability of the knee may be a consequence of cartilage or ligament damage. Further injury to the joint may occur if the problem is left untreated, along with an increased risk of arthritis.
Complete knee replacement is now a successful option but, in many cases, arthroscopic (keyhole) surgery and physiotherapy can give your knee a new lease of life and delay or prevent the need for such surgery. You are welcome to contact us to arrange a consultation.
![]()
Restoring Connective Tissue

We mentioned one ligament in relation to the patella, although more are involved in the knee's function, such as the anterior cruciate ligament. An area where even professional athletes can benefit from:
